Wide Regular QRS Tachycardia: VT vs. SVT
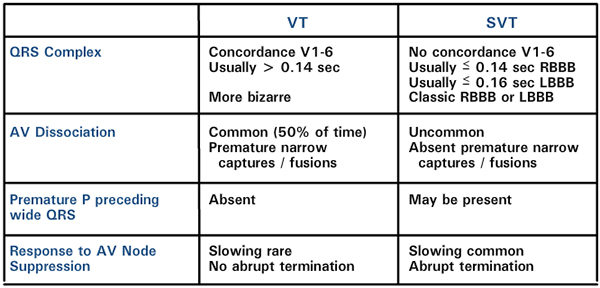
When evaluating a wide regular QRS tachycardia, there are several important differentiating factors for ventricular tachycardia (VT) versus supraventricular tachycardia (SVT).
First, characteristics of the QRS complex. Concordance of the QRS in V1-6, i.e., all of the QRS’ are positive or negative, is considered pathognomonic for ventricular tachycardia. In SVT the QRS is usually less than 0.14 sec. for right bundle branch block and less than 0.16 sec. for left bundle branch block; in VT usually the QRS width is greater than 0.14 sec. In SVT with aberration, a classic RBBB or LBBB is typical, whereas in VT the appearance is more bizarre.
Next, P wave relationships: AV dissociation occurs in 50% of ventricular tachycardias but may be difficult to diagnose without an atrial lead. AV dissociation (that is, independent atrial and ventricular rhythms) or premature narrow QRS complexes (capture or fusion beats) are considered pathognomonic of VT. Absence of premature P waves preceding a wide QRS is more suggestive of VT.
Lastly, response to AV nodal suppression. Slowing of the QRS rate, is common with SVT and rare with VT; abrupt termination with adenosine or vagal stimulation (e.g. carotid sinus massage) is virtually pathognomonic for SVT.